Introduction: Therapy-related myeloid neoplasms (t-MN) are associated with extremely poor clinical outcomes in otherwise long-term cancer survivors. t-MN accounts for ~20% of cases of myeloid neoplasms and is expected to rise due to the increased use of chemotherapy/radiotherapy (CT/RT) and improved cancer survivorship. Historically, t-MN was considered a direct consequence of DNA damage induced in normal hematopoietic stem cells (HSC) by DNA damaging cytotoxics. However, these studies have largely ignored the bone marrow (BM) microenvironment and the effects of age and concurrent/previous cancers.
Aim: We performed an exhaustive functional study of mesenchymal stromal cells (MSC) obtained from a comparatively large cohort of t-MN patients and carefully selected control populations to evaluate the long-term damage induced by cytotoxic therapy to BM microenvironment and its impact on malignant and normal haematopoiesis.
Methods: Four different cohorts were used: (1) t-MN, in which myeloid malignancy occurred after CT/RT for a previous cancer (n=18); (2) patients with multiple cancer and in which a myeloid neoplasm developed following an independent cancer which was not treated with CT/RT (MC-MN; n=10); (3) primary MN (p-MN; n=7) untreated and without any prior cancer or CT/RT; (4) age-matched controls (HC; n=17). Morphology, proliferation, cellular senescence, differentiation potential and γH2AX DNA damage response was performed. Stem/progenitor supportive capacity was assessed by co-culturing haematopoietic stem cells on MSC feeder-layer in long-term culture initiating assay (LTC-IC). Cytokine measurements were performed using 38-plex magnetic bead panel (Millipore) and RNA sequencing libraries were prepared with Illumina TruSeq Total RNA protocol for 150bp paired-end sequencing on a NextSeq500 instrument. Functional enrichment analysis was performed using EnrichR software.
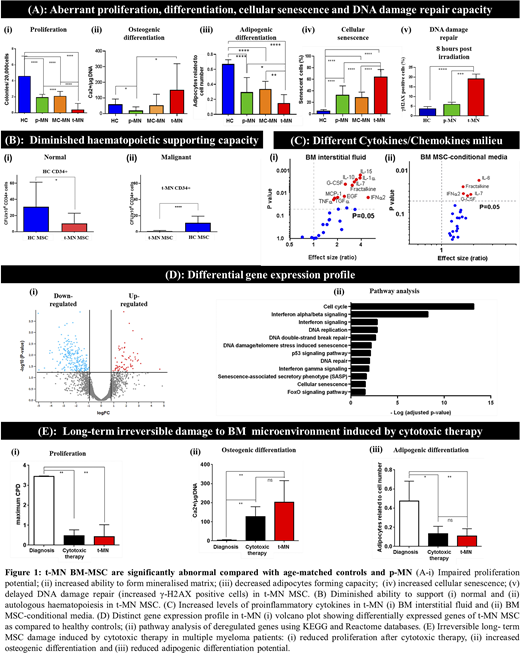
Results: MSC cultured from t-MN patients were significantly different from HC, p-MN and MC-MN MSC according to multiple parameters. They exhibited aberrant morphology consisting of large, rounded and less adhesive cells compared to typical spindle-shaped morphology observed with controls. MSC from myeloid neoplasm also showed impaired proliferation, senescence, osteo- and adipogenic differentiation with t-MN MSC showing the greatest differences. DNA repair was dramatically impaired compared to p-MN and HC (Fig.1A). Importantly, these aberrant t-MN MSC were not able to support normal or autologous in vitro long-term haematopoiesis (Fig.1B).
The biological characteristic and poor haematopoietic supportive capacity of MSC could be "cell-intrinsic" or driven by an altered paracrine inflammatory microenvironment. Interestingly, several inflammatory cytokines were higher in t-MN compared with marrow interstitial fluid obtained from p-MN patients (Fig.1Ci) and many of these including Fractalkine, IFNα2, IL-7 and G-CSF were also significantly higher in t-MN MSC conditional media (Fig.1Cii). Together, this data suggest that t-MN microenvironment is distinct from p-MN with paracrine production of pro-inflammatory milieu that may contribute to poor HSC supportive capacity.
Preliminary whole transcriptome analysis revealed differential gene expression between t-MN and HC (Fig.1Di) and p-MN MSC. Importantly, the deregulated genes play critical role in cell cycle, DNA damage repair, and cellular senescence pathways explaining phenotypical characteristic of t-MN MSC (Fig.1Dii). Moreover CXCL12 expression, a key regulator of haematopoiesis, was significantly lower in t-MN compared to HC (p=0.002) and p-MN MSC (p=0.009), thus explaining poor HSC supportive capacity.
The key difference between the p-MN, MC-MN and t-MN is prior exposure to CT/RT. To study this we obtained MSC from two t-MN patients for whom we had samples at the time of their primary cancer, post high-dose chemotherapy and at the time of t-MN. MSC displayed aberrant proliferation and differentiation capacity after high-dose cytotoxic therapy (2 to 4 years prior to developing t-MN) and remained aberrant at t-MN diagnosis (Fig.1E).
Conclusions: BM-MSC from t-MN patients are significantly abnormal compared with age-matched controls and typical myeloid neoplasm. Importantly, prior CT/RT leads to long-term irreversible damage to the BM microenvironment which potentially contributes to t-MN pathogenesis.
Hughes:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; BMS: Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding. Hiwase:Novartis Australia: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal